Clinical Trial Management
Plan. Execute. Analyze.
Study planning, site management, patient enrollment, and trial execution. Run clinical trials with the same rigor you apply to manufacturing.
The trial that couldn't find its data.
FDA inspection of a Phase III trial. Auditor asks for the monitoring visit report from Site 23, Visit 4. The CRA documented it—somewhere. The TMF is scattered across SharePoint, email attachments, and a legacy eTMF that nobody likes using.
Four hours later, the document surfaces. It was misfiled. The finding: "Trial Master File is not maintained in a manner that allows timely retrieval of essential documents."
Clinical trials generate enormous documentation. If you can't find it, you might as well not have it.
Study planning that scales
A Phase III trial: 150 sites, 12 countries, 2,000 patients, 36-month enrollment. The protocol is just the beginning. Site budgets, IRB submissions, regulatory filings, investigator agreements, monitoring plans, data management plans—each requiring coordination across teams and geographies.
Seal structures study planning as interconnected workstreams. Protocol drives everything else. Site selection criteria feed feasibility. Country requirements determine regulatory strategy. Milestones link across workstreams so delays in one area surface impacts to others.
You see the whole trial, not just your piece of it.
Site management from feasibility through close-out
Sites are your partners—and your biggest variable. Selection, qualification, initiation, enrollment performance, protocol compliance, close-out. Each site has its own trajectory.
Seal tracks sites through their lifecycle. Feasibility questionnaires score against criteria. Site initiation visits have checklists and required documents. Enrollment targets track against actuals. Protocol deviations aggregate to site-level metrics. Problem sites surface before they become critical.
When a site underperforms, you see it early enough to act.
Enrollment that predicts and adapts
Will you hit enrollment targets? When? Most enrollment tracking is backward-looking—you know you're behind after you're behind.
Seal models enrollment dynamically. Current site performance, upcoming site activations, seasonal patterns, competitive trials. The model updates as reality unfolds. If you're trending to miss your target, you know months in advance—enough time to add sites or adjust expectations.
Monitoring visits with purpose
CRAs conduct monitoring visits. They check source data, review consent forms, verify drug accountability, address site questions. Each visit generates findings and action items.
Seal structures monitoring visit workflow. Pre-visit planning identifies focus areas. Visit checklists ensure consistency. Findings capture with severity and required action. Follow-up tracks to closure. The monitoring report generates from structured data—no report writing from scratch.
Monitoring becomes a system, not a heroic individual effort.
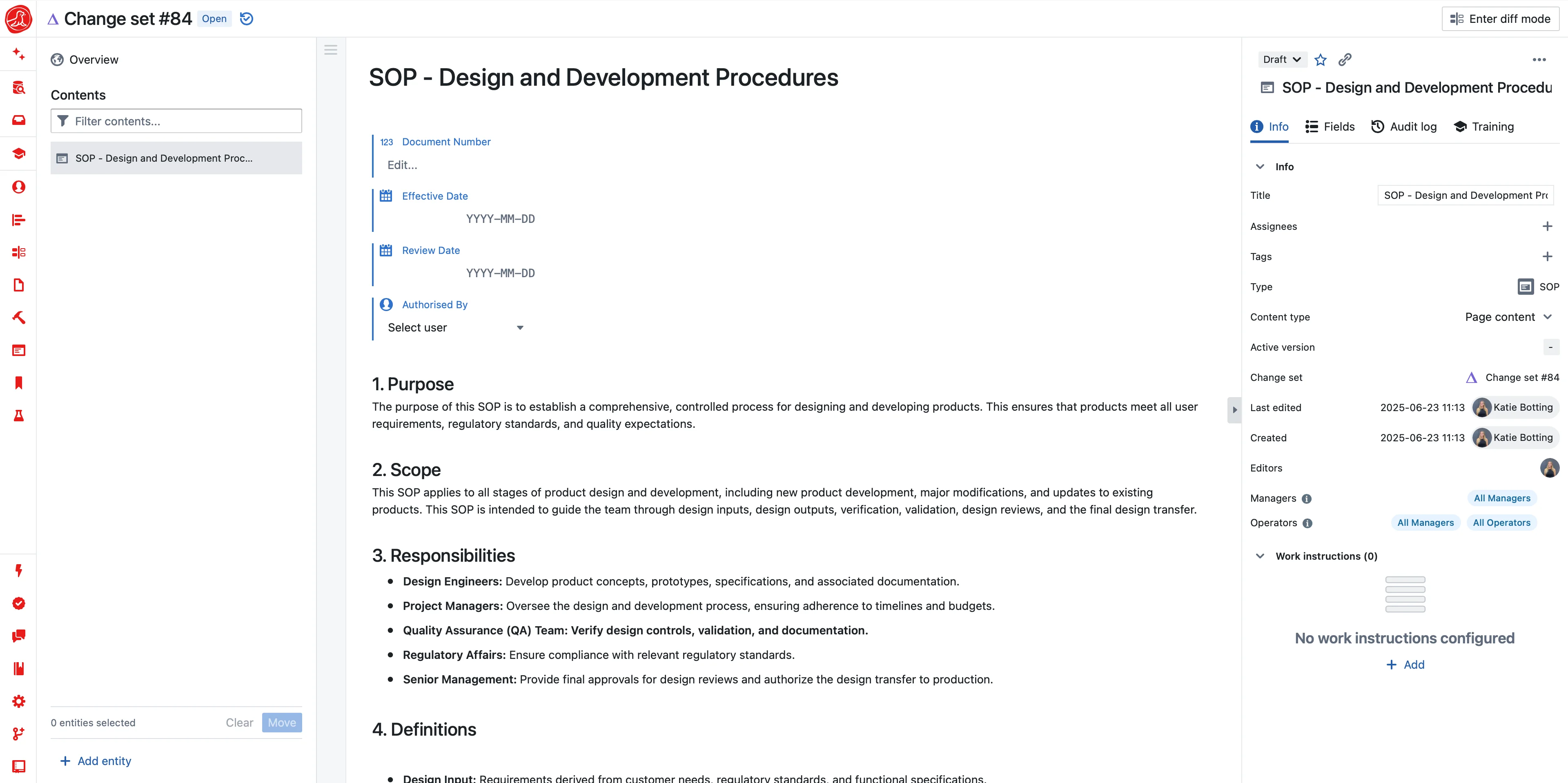
Trial Master File that's always inspection-ready
TMF is the evidence of trial conduct. ICH E6 requires it. Inspectors expect it. Most TMFs are disasters.
Seal maintains TMF continuously. Documents file to the TMF structure (DIA reference model or your own) as they're created. Expected documents track against actual. Completeness metrics show gaps before inspectors find them.
When the auditor asks for a document, retrieval is seconds—not hours or days.
Safety reporting integrated with PV
SAEs in clinical trials have reporting requirements. Expedited reports to IRBs and regulators. Safety data that feeds benefit-risk assessment. SUSARs that affect all sites on the protocol.
Seal integrates clinical safety with pharmacovigilance. SAE reports flow through the same case management system as post-market events. Investigators receive safety notifications through the system. DMC reports generate from accumulated data.
Safety doesn't live in a separate silo—it's part of the clinical platform.
Regulatory submissions and approvals
IND/CTA submissions. Protocol amendments. Annual reports. Each country has its own requirements and timelines.
Seal tracks regulatory submissions by country. Initial filings, approval status, amendment submissions, annual reports. When you amend the protocol, the system identifies which countries need updated filings and tracks completion.
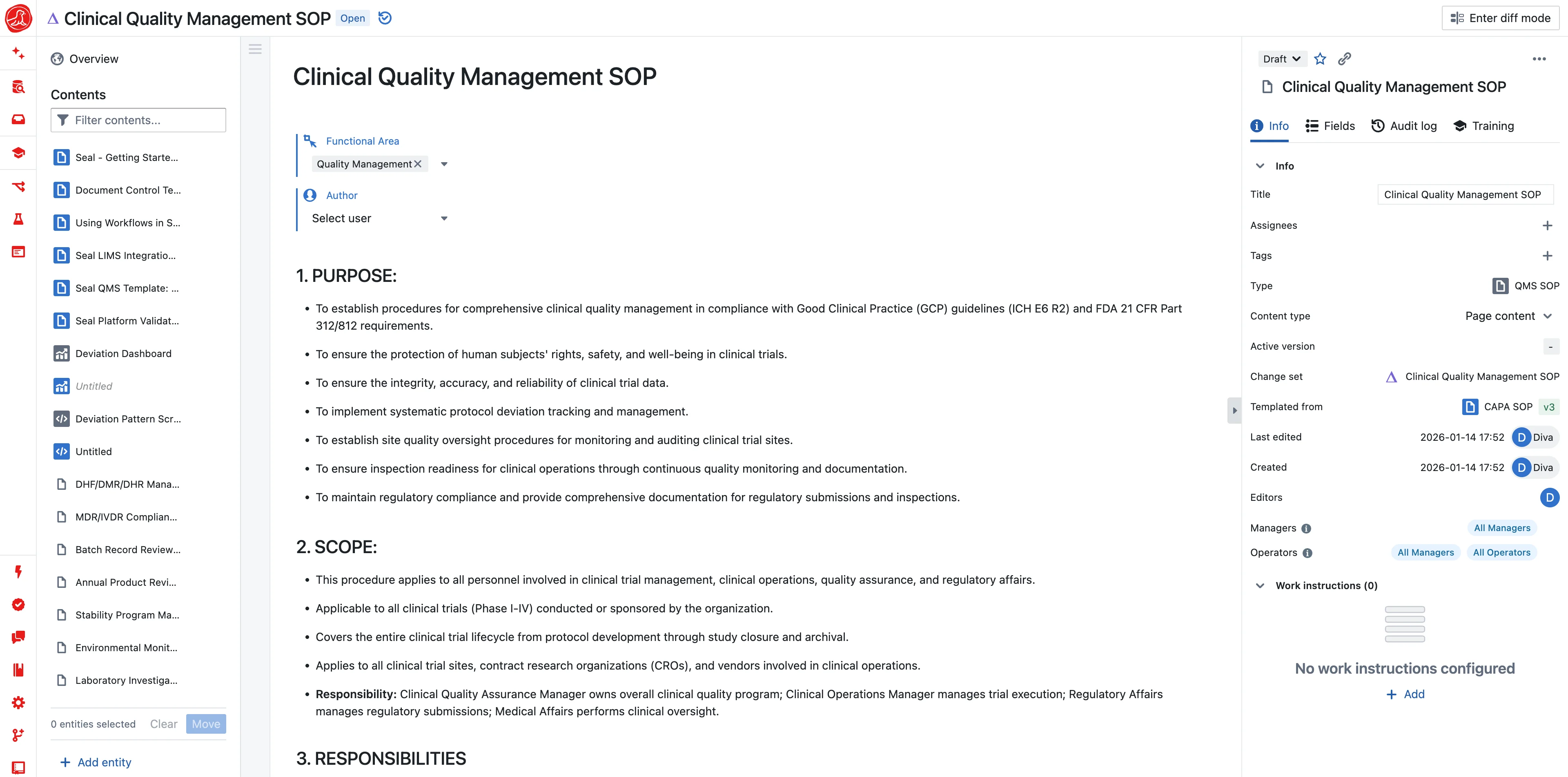
Data quality and issue management
Protocol deviations. Data queries. Site issues. Quality events. Clinical trials generate quality issues constantly.
Seal manages clinical quality with the same rigor as manufacturing quality. Deviations classify and trend. Root causes analyze. Corrective actions track. Quality metrics roll up to study level and portfolio level.
When you report to the safety monitoring board, quality data is ready.
Capabilities