Clinical Quality Assurance (CQA) plays a crucial role in clinical trials and healthcare. It involves different practices and tools aimed at making sure clinical research and healthcare services follow high quality standards. Effective CQA is essential for protecting patient safety, the reliability of clinical trial data, and regulatory compliance. This guide explains what CQA is, key roles involved and best practices. Whether you're an experienced professional or new to the field, this guide will help you excel in ensuring clinical quality.
What is Clinical Quality Assurance?
Definition
Clinical Quality Assurance (CQA) refers to the systematic processes and procedures adopted to make sure that clinical trials and healthcare practices meet high standards of quality. This involves planning, managing, and executing quality control procedures to check data integrity, regulatory compliance, and the safety and well-being of patients. CQA includes a wide range of processes like audits, inspections, training, as well as developing standard operating procedures (SOPs).
Why is CQA important?
Clinical Quality Assurance matters for a few primary reasons.
- Protecting patients: Ensures patient safety in clinical trials.
- Ensuring reliable data: Guarantees data accuracy and credibility.
Key components of clinical quality assurance
Compliance
As we covered already, clinical quality assurance plays a pretty essential role in making sure that clinical trials and healthcare practices meet the regulatory requirements set by various health authorities.
These regulatory bodies set guidelines and standards for the safety, efficacy, and ethical conduct of clinical trials. Here are a few of the main aspects of clinical quality assurance:
- Adherence to guidelines
CQA involves making sure that all clinical trial activities are conducted in adherence with regulatory guidelines like Good Clinical Practice (GCP). - Documentation & reporting
For clinical trials, it's important to have detailed documentation and timely reporting of trial data. CQA systems enable the proper recording of trial procedures and outcomes, ensuring that all necessary documentation is complete, accurate, and available for regulatory review. - Audits and inspections
Audits help identify and correct compliance issues before they become larger issues, helping follow regulatory standards. CQA prepares organisations for external inspections by regulatory bodies, so that they can get approval and continuation of their clinical trials.

Data integrity
Data integrity involves maintaining the accuracy and completeness of data throughout its life cycle. This helps make informed decisions based on clinical trial outcomes.
In the context of CQA, this means:
Accurate data collection
Standardised procedures help reduce errors with consistency.
- Train staff on proper data entry techniques
- Validated tools for electronic data capture (EDC) systems
- Regular Checks and audits conducted to ensure data accuracy
Validation and verification
Regular validation and verification usually includes:
- Cross-checking data entries with source documents
- Statistical analyses to detect anomalies through statistical checks
- Periodic reviews verify data accuracy.
To illustrate this, in a Phase III trial, validation would include cross-referencing patient records with EDC entries and performing statistical checks for data integrity.
Audit trails
Audit trails provide transparency and track data changes.
- Detailed, chronological records of all data modifications
- Compliance with FDA and EMA requirements is ensured through transparent audit trails.
For example, during an FDA inspection the clinical trial team would provide EDC audit trails showing records of data entries and modifications.
Patient safety
The cornerstone of clinical quality assurance is, of course, patient safety. CQA helps maintain high standards of patient care in a few main ways.
Risk assessment and management
CQA involves proactively spotting risks at the trial design stage. Predicting potential adverse effects and setting up mitigation strategies, helps prioritise patient safety from the outset.
Adverse event monitoring
Continuous monitoring of patient health is essential to detect and respond to adverse events swiftly. Real-time data collection and analysis allow for immediate intervention when necessary, ensuring that any adverse effects are promptly addressed.
Ethical considerations
Ethical practices are integral to CQA, ensuring that patient rights and well-being are protected. This includes obtaining informed consent from participants and maintaining strict confidentiality of patient data.
Example: Participants are fully informed about the trial, including potential risks and benefits, and their consent is obtained voluntarily. Confidentiality of their data is rigorously maintained.
Best Practices in Clinical Quality Assurance
Standard Operating Procedures (SOPs)
Standard Operating Procedures (SOPs) help guide clinical trials and make sure that all processes are carried out consistently. SOPs provide detailed, written instructions on how to perform specific procedures, helping to standardise operations across different teams and sites.
Here are a few of the main ways the SOPs help in the context of clinical trials:
- Consistency and standardisation
- Regulatory compliance e.g. GCP guidelines
- Quality control
- Training and onboarding
We created a useful SOP Template here to make sure all your processes are standardised.
Training & education
Ongoing training and education for staff involved in clinical trials are crucial for maintaining high standards of quality and promoting the safety and efficacy of the trials. Continuous professional development helps staff stay updated with the latest guidelines, technologies, and best practices. This can be done by keeping up with regulatory changes, regularly offering training and training resources to staff and actively trying to improve performance of teams.
If you're looking for a useful resource for managing training, you can use this Training Management template.
Risk management
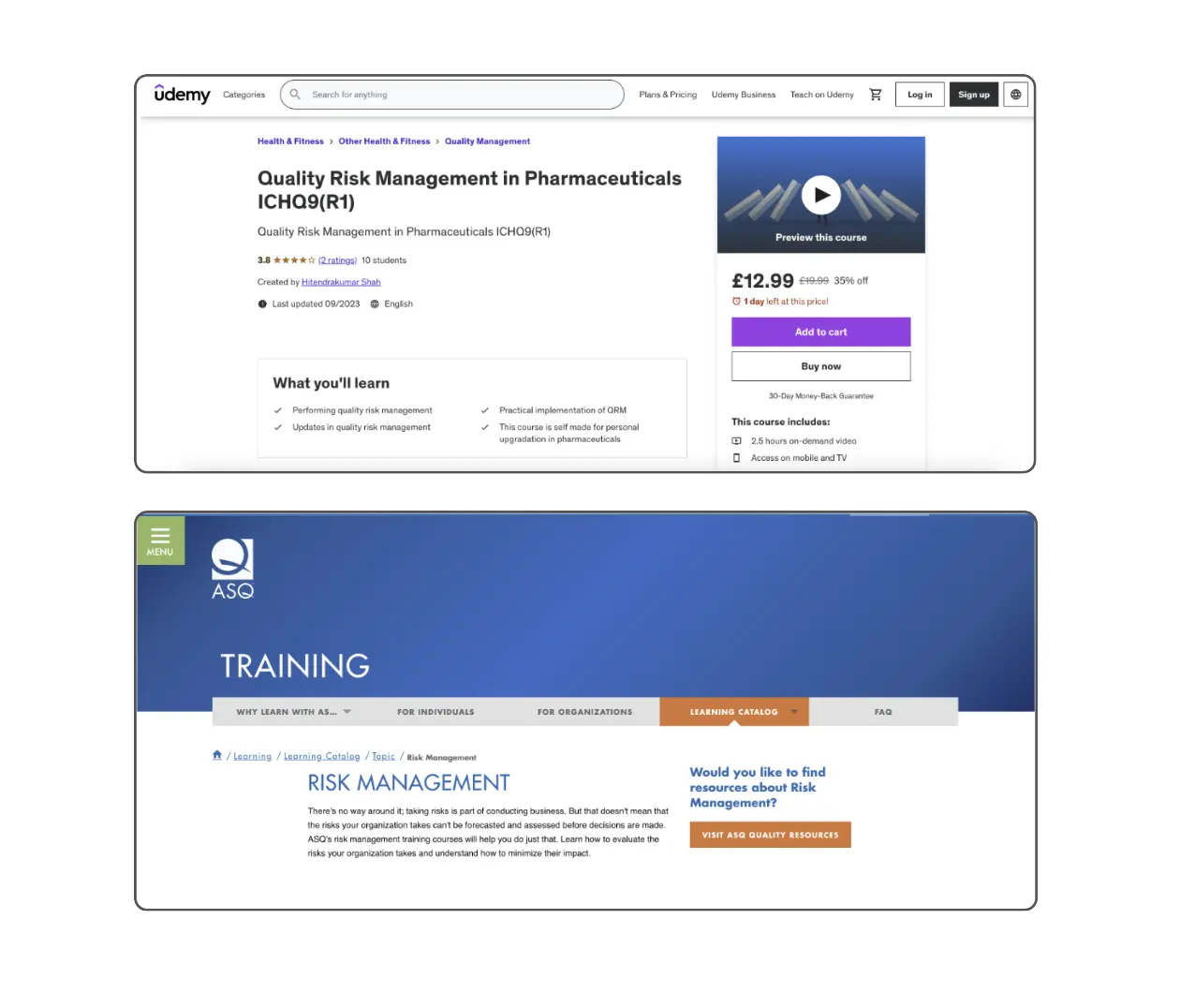
Risk management needs to be part of the framework when planning a clinical study. Proactive risk management strategies help ensure the safety of participants and the integrity of trial data. Risk management can be boiled down to two parts: identifying risks and then coming up with mitigation strategies for said risks.
We've put together a list of 11+ compliance and risk management courses for quality assurance managers, if you're interested in learning risk management best practices.
Auditing and monitoring
Regular audits and monitoring are integral to maintaining high standards of quality and compliance in clinical trials. These activities help ensure that all trial processes adhere to regulatory requirements and internal quality standards.
- Internal audits: reviewing the effectiveness of processes, making sure SOPs are being followed correctly.
- External audits: an independent auditor or regulatory body provides objective assessment of a trial's compliance with standards.
- Reporting and documentation: detailed reports with clear records of findings and corrective actions taken, which can be reviewed by regulatory authorities.
Functions and responsibilities in clinical quality assurance
Clinical Quality Assurance Officer
A Clinical Quality Assurance Officer ensures that clinical trials maintain high standards of quality and comply with regulatory guidelines. They are responsible for developing procedures, training staff, and monitoring trial activities to ensure consistency and adherence to standards.
Responsibilities:
- Developing SOPs
- Train staff
- Monitoring compliance
- Managing risks
- Conducting audits
Quality Assurance Auditor
Quality Assurance Auditors provide an independent assessment of clinical trials to ensure they meet regulatory standards and internal quality guidelines. They conduct systematic audits, document findings, and recommend corrective actions to maintain compliance and quality.
Responsibilities:
- Conducting audits
- Evaluating compliance
- Documenting findings
- Implementing corrective actions
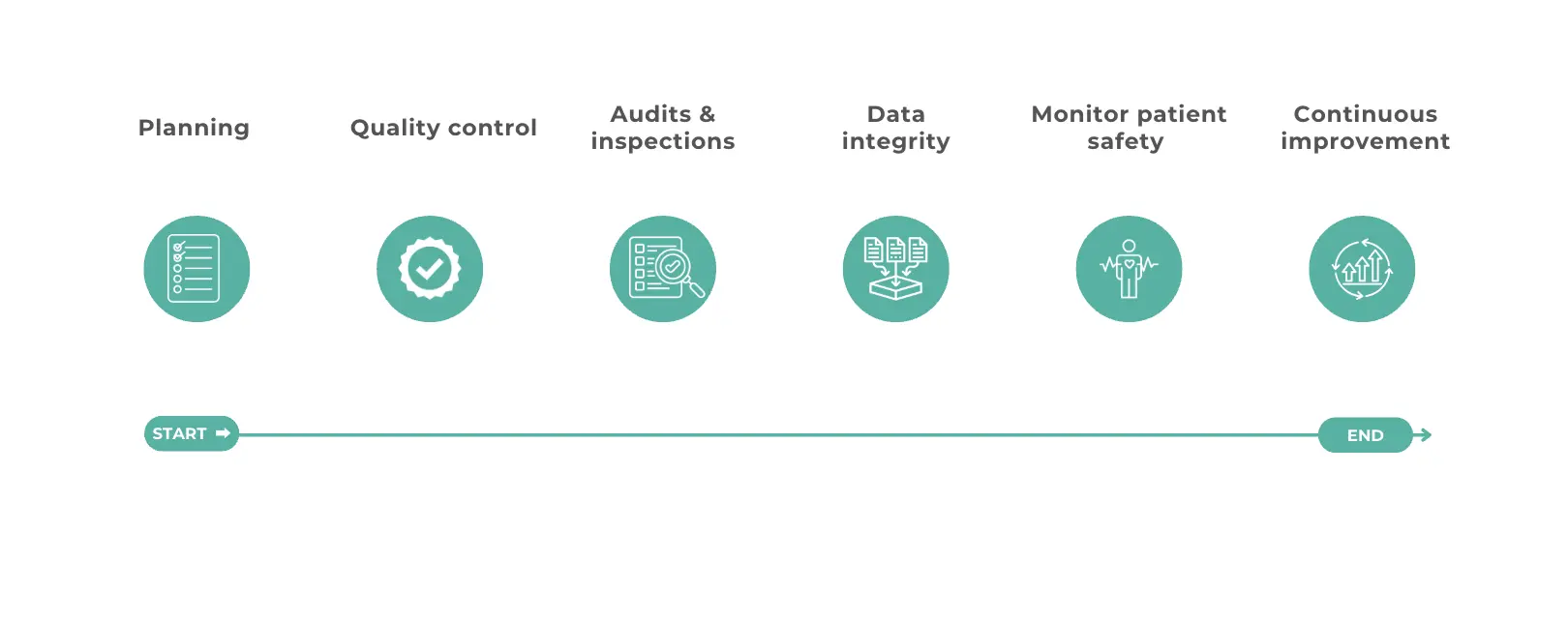
Implementing a clinical quality assurance program
Implementing a clinical quality assurance program is critical to ensure the success and integrity of clinical trials. Here's a step-by-step guide to help you develop, execute, and continuously improve your CQA program.
Planning & development
To start, you need a solid plan. Here's how to get going:
- Define objectives
- Establish SOPs
- Allocate resources e.g. personnel, tools, and budget
- Regulatory framework ie. align your CQA program with regulatory guidelines, e.g. FDA, EMA, and ICH GCP standards.
Execution & monitoring
Once a plan is made, effective execution and continuous monitoring are key:
- Training: conduct training sessions for all staff involved in the clinical trial to ensure they understand CQA procedures.
- Data collection & management: systems to ensure data accuracy and integrity.
- Real-time monitoring: use tools to track trial progress and find potential issues early.
- Regular audits: review compliance with SOPs and identify areas for improvement.
Continuous improvement
To keep your CQA program effective, set up a feedback loop to gather input from staff and participants, and make adjustments. Try to regularly review the program and make improvements. For example, after completing a clinical trial, the QA team gathers feedback from participants and staff, reviews the program's performance, updates SOPs based on the latest EMA guidelines.

